What is Ergonomics?
Ergonomics is the study of designing and arranging products, systems, and environments in a way that optimizes human well-being, safety, and performance. It aims to reduce discomfort, injuries, and stress while increasing efficiency, productivity, and satisfaction.
Ergonomics is especially crucial in workplaces where individuals perform repetitive tasks or spend long hours in static positions, as it can help prevent musculoskeletal disorders and other work-related injuries. Now we will know about ergonomics in work place.
Table of Contents
Office Ergonomics
Office ergonomics is important because it can help prevent work-related injuries and improve overall well-being and productivity of office workers. By designing workstations, chairs, and other equipment in a way that promotes good posture and reduces physical strain, employers can reduce the risk of repetitive stress injuries, back pain, and other musculoskeletal disorders.
Proper office ergonomics can also help to reduce eye strain, headaches, and other discomfort associated with computer work.
Some common disorders among office employees:
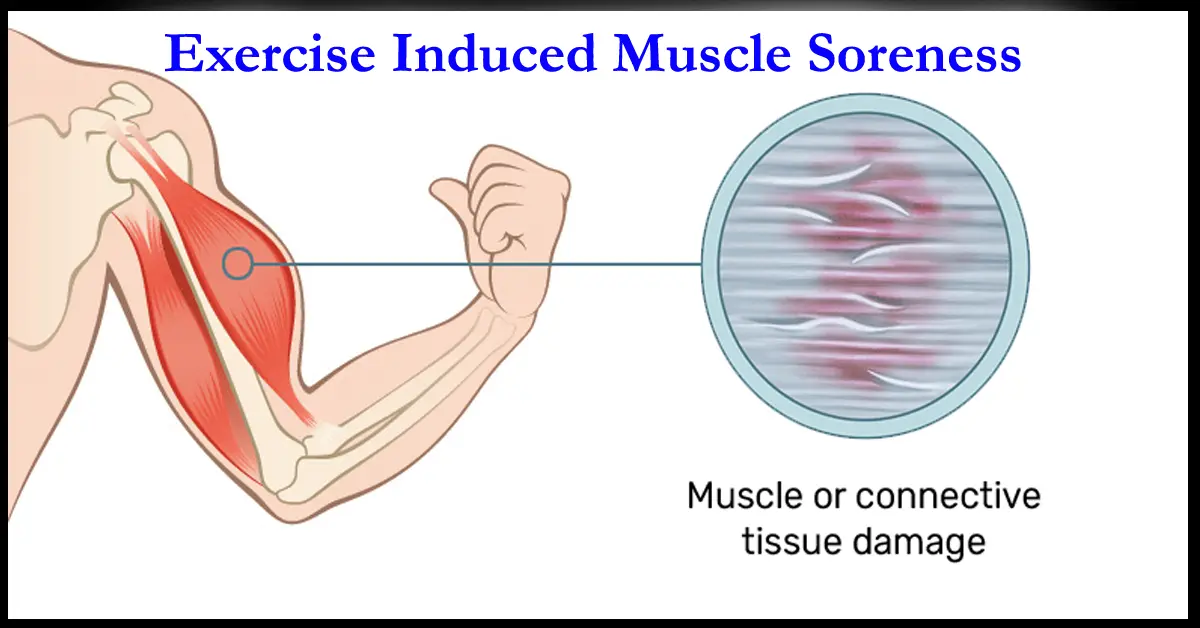
Injury to the muscle and skeletal system is called Musculoskeletal disorders (MSDs). MSDs which occur due to some specific work are called Work related musculoskeletal disorders (WRMSDs).
WRMSDs are common among office employees and can be caused by prolonged sitting or standing, repetitive motions, awkward postures, and insufficient rest breaks. Some of the most common MSDs experienced by office employees include:
- Carpal tunnel syndrome
- Tendinitis
- Trigger finger
- Tennis elbow
- Rotator cuff injuries
- Disc herniation
- Repetitive strain injuries (RSIs) etc.
Some common symptoms of above MSDs are:
- Neck and shoulder pain: Incorrect posture can cause strain on the neck and shoulders, leading to pain and stiffness.
- Back pain: Poor posture can cause back pain, particularly in the lower back, by putting undue stress on the spinal column.
- Headaches: Tension in the neck and shoulders can cause tension headaches.
- Eye strain: Poor posture can cause eye strain by forcing you to tilt your head or lean forward to see the computer screen.
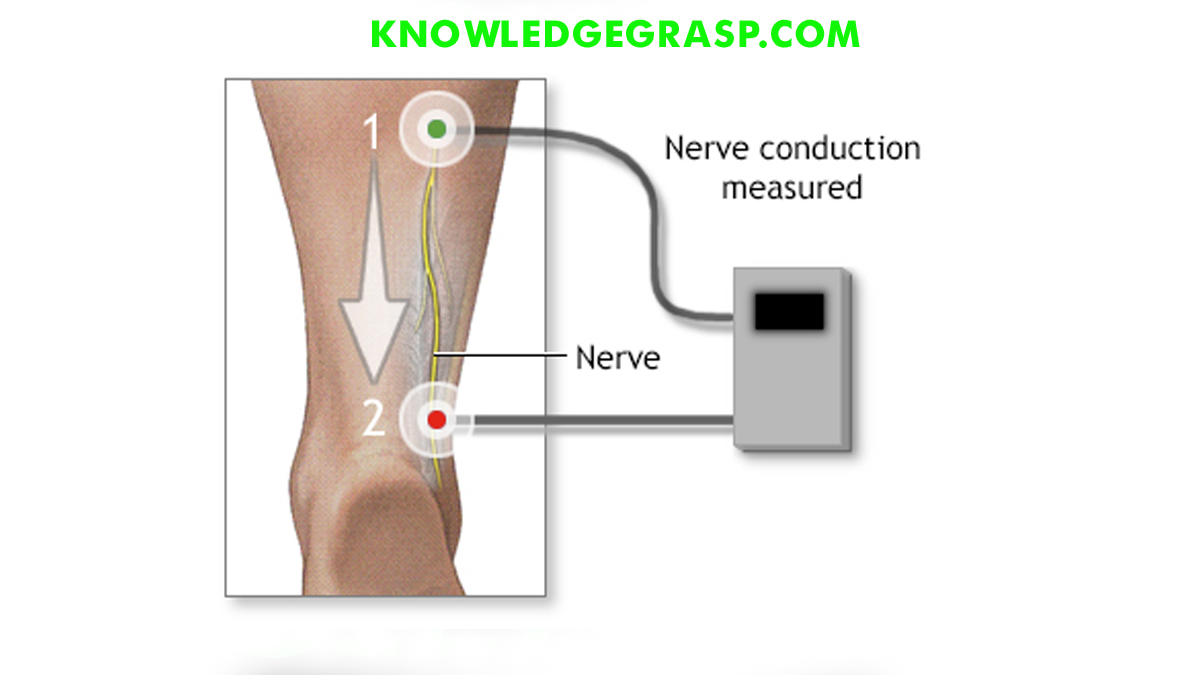
- Tingling and numbness: Poor posture can put pressure on nerves in the arms and legs, leading to tingling and numbness.
- Fatigue: Poor posture can lead to fatigue, particularly in the neck and shoulders.
Long-term effects of WRMSDs
If the above symptoms are left untreated the office workers can experience chronic pain, reduced range of motion, decreased muscle strength, and decreased overall quality of life. If left untreated, MSDs can lead to long-term disability, reduced work productivity, and increased healthcare costs.
Repetitive strain injuries (RSIs) such as carpal tunnel syndrome, tendinitis, and tennis elbow can result in chronic pain, reduced grip strength, and reduced hand function. Neck and back pain caused by poor ergonomic practices can lead to chronic pain, limited mobility, and a decreased quality of life.
In addition to the physical effects, long-term MSDs can also lead to psychological stress and mental health issues such as anxiety and depression. This can further impact an employee’s work productivity and quality of life.
Employers can prevent or reduce the long-term effects of MSDs by implementing ergonomic interventions such as providing ergonomic assessments, training on proper posture and stretching techniques, and offering appropriate equipment and workstations. Prompt treatment and rehabilitation of MSDs can also help reduce the risk of long-term effects.
Benefits of following ergonomics:
- Increased comfort: Ergonomic design can help reduce discomfort, fatigue, and pain associated with prolonged sitting or standing.
- Improved productivity: If employees follow ergonomics it can improve work efficiency, accuracy, and speed.
- Reduced injury risk: Ergonomic design can reduce the risk of musculoskeletal disorders and other workplace injuries.
- Better posture: Ergonomic design can help promote good posture, which can reduce the risk of neck and back pain.
- Improved employee morale: Providing an ergonomic workspace can improve employee satisfaction, leading to higher morale and job satisfaction.
- Cost savings: Implementing ergonomic design can lead to cost savings by reducing absenteeism, turnover, and workers compensation claims.
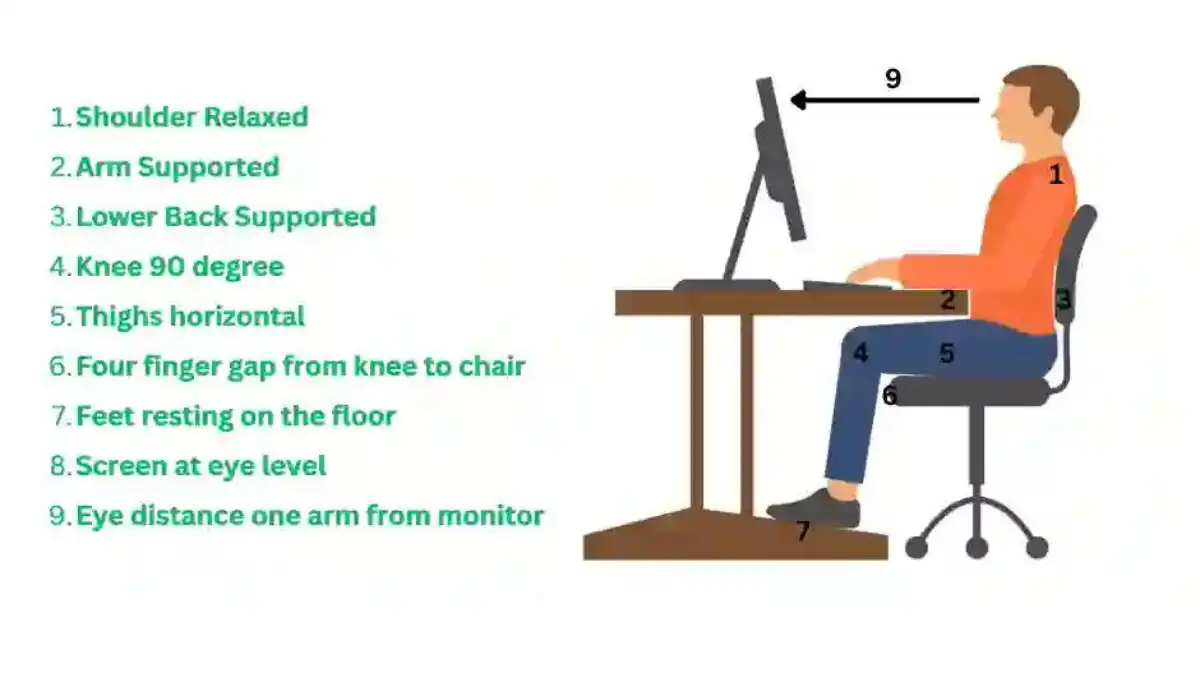
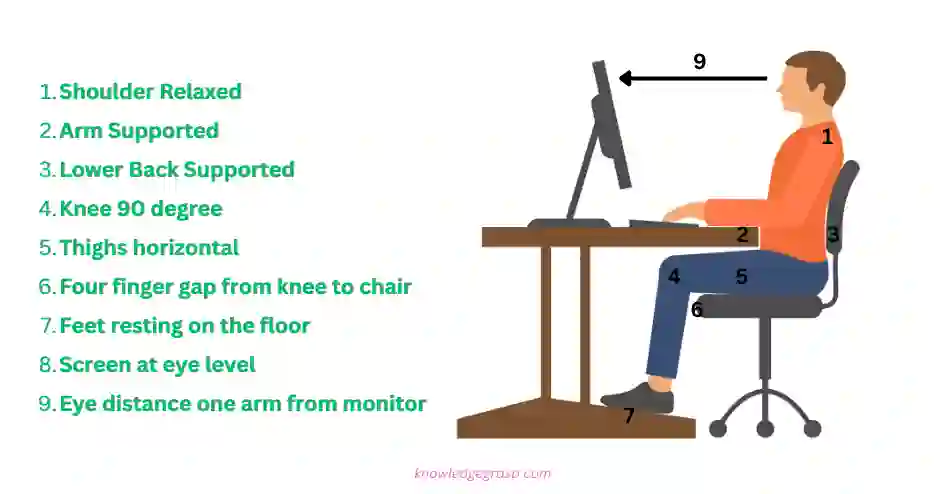
Here are some tips for an ergonomic office setup:
- Chair: Use a chair with adjustable height, backrest, and armrests. Ensure that your feet are flat on the floor and your hips are level with or higher than your knees. Adjust the backrest to support your lower back.
- Desk: Use a desk with adjustable height that allows your forearms to rest comfortably on the desk and your wrists to be straight while typing. Position your computer monitor at eye level, an arm’s length away from your body.
- Keyboard and Mouse: Use an ergonomic keyboard and mouse to reduce strain on your hands and wrists. Keep the keyboard and mouse at the same level and close to your body to avoid reaching and straining.
- Lighting: Use proper lighting to avoid eye strain and reduce glare on the computer screen. Use task lighting to illuminate specific work areas.
- Posture: Sit up straight with your shoulders relaxed and your head level. Avoid slouching or leaning forward.
- Breaks: Take frequent breaks to stand up, stretch, and move around. This can help reduce the risk of fatigue and strain.
By setting up your office ergonomically, you can help reduce the risk of musculoskeletal disorders (MSDs) and improve your work efficiency and productivity.
Stretching exercises in work place
Stretching exercises can be helpful in reducing muscle tension, increasing blood flow, and improving flexibility, particularly for individuals who spend extended periods sitting in front of a computer. Here are some stretching exercises that can be done in an office setting:
- Neck stretch: Gently tilt your head to one side, bringing your ear toward your shoulder. Hold for 10-15 seconds and repeat on the other side.
- Shoulder roll: Roll your shoulders forward and backward in a circular motion for 10-15 repetitions.
- Seated spinal twist: While seated, cross one leg over the other and twist your torso toward the leg that is crossed. Place your opposite hand on the outer thigh and hold for 10-15 seconds. Repeat on the other side.
- Hamstring stretch: While seated, extend one leg straight out and reach for your toes. Hold for 10-15 seconds and repeat on the other side.
- Wrist stretch: Hold your arm out in front of you with your palm facing down. Use your opposite hand to gently pull your fingers back toward your wrist. Hold for 10-15 seconds and repeat on the other side.
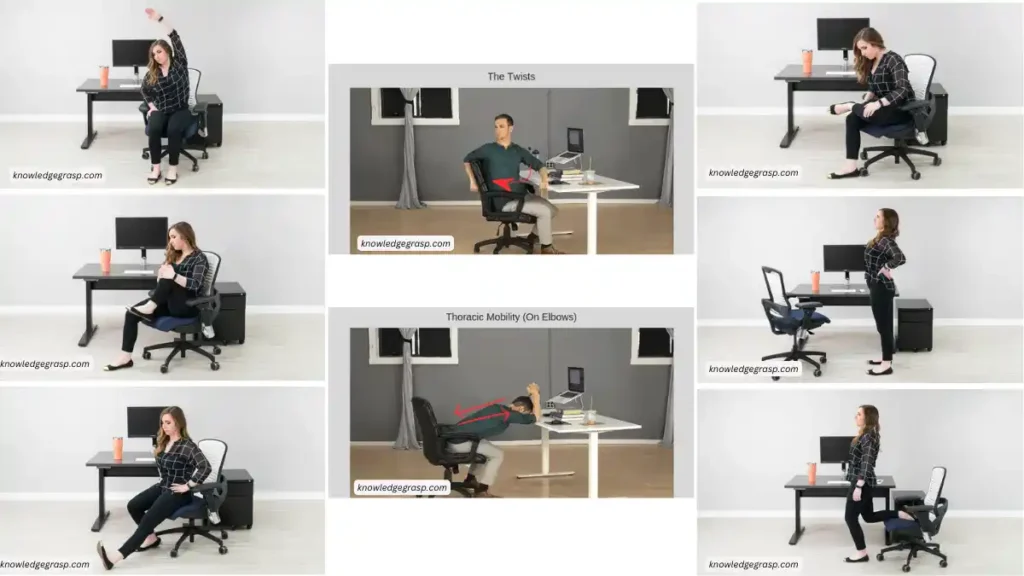
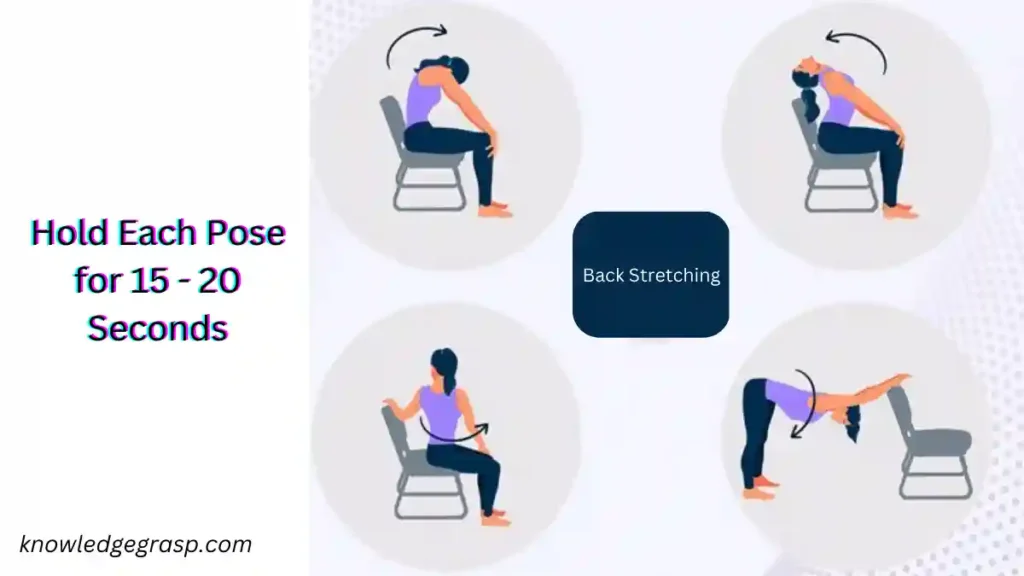
Here are some stretching exercises for low back pain that can be done in the office:
- Seated forward fold: Sit in your chair with your feet flat on the floor. Slowly fold forward from your hips, reaching toward your feet or the floor. Hold for 10-15 seconds and slowly return to a seated position.
- Figure four stretch: Sit in your chair and cross one ankle over the opposite knee. Gently press down on the crossed leg until you feel a stretch in your buttocks and lower back. Hold for 10-15 seconds and repeat on the other side.
- Seated twist: Sit in your chair with your feet flat on the floor. Twist your torso to one side, holding the back of your chair for support. Hold for 10-15 seconds and repeat on the other side.
- Cat-cow stretch: Sit on the edge of your chair with your feet flat on the floor. Place your hands on your thighs and arch your back, tucking your chin into your chest. Then slowly round your back, dropping your head forward. Repeat for 10-15 repetitions.
- Hip flexor stretch: Sit on the edge of your chair with one knee bent and the other leg extended behind you. Gently press your hips forward until you feel a stretch in your hip flexor. Hold for 10-15 seconds and repeat on the other side.
- Back extension: Stand in your place and keep both hands on your lower back for support. Lean backward and hold the position for 15-20 seconds and repeat every one hour.
Ergonomics in work place( Do’s & Don’ts )